Donnie Allison Grand Marshal for Georgetown Speedway’s Melvin Joseph Memorial
GEORGETOWN – NASCAR Hall of Famer Donnie Allison, a 10-time winner in stock car racing’s top series who may be best remembered for his final lap, backstretch brawl with Cale Yarborough in …
-
-
Gubernatorial candidate Matt Meyer unveils plan to improve education in Delaware
WILMINGTON — New Castle County Executive and gubernatorial candidate Matt Meyer has unveiled a comprehensive, 23-page education plan that …
-
-
-
Delaware's June Jam CEO, founder Hartley dead at 68
Bob Hartley, CEO and president of the June Jam charity music festival, died in his sleep Sunday.
-
-
-
Dover shooting incident brings murder charge
A 23-year-old Dover man was arrested and charged with murder following a shooting incident Sunday, authorities said. Police said officers …
-
-
The annual municipal election in Harrington scheduled May 7 has been canceled, due to a lack of contested races.


View this issue of The Delaware State News or browse other issues.
Disclosure
-
-
Merlet: Inspector general bill could move forward Wednesday
On Wednesday, the Delaware Senate’s Executive Committee has the opportunity to do something great: It can release the inspector general bill …
-
-
-
Speak Up: A global treaty on plastics can help us all
Susan Bass shared an Opinion on Monday about the start of the fourth round of negotiations for a global plastics treaty.
-
-
-
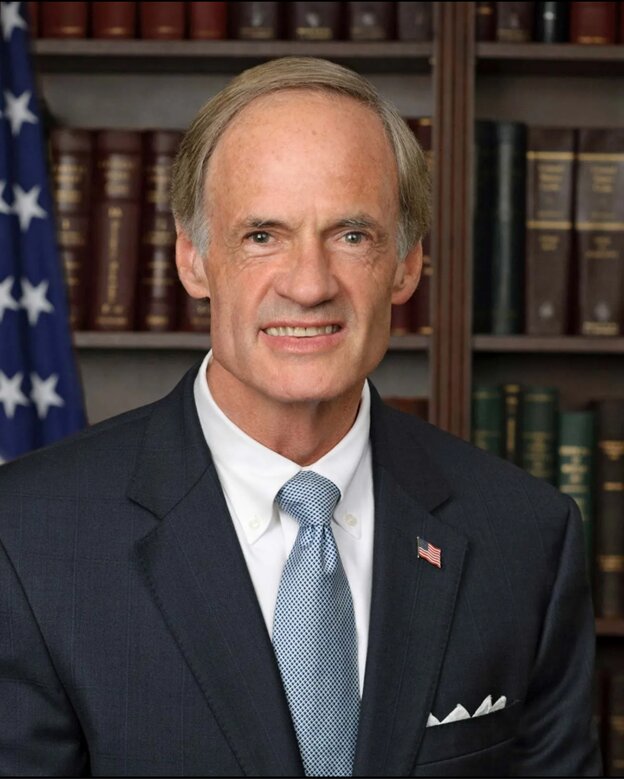
Speak Up: Blunt Rochester sets Delaware fundraising record for federal candidates
During the first quarter of 2024, Congresswoman Lisa Blunt Rochester raised more than $1 million in her race to represent Delaware in the U.S. …
-
-
Downtown Milford roadwork affecting business
With growth comes some growing pains, and right now, downtown Milford business owners are feeling them. Due to ongoing road construction, travel has been hampered through one of the busiest retail districts in the city.



Harrington Raceway harness racing results, entries

Caesar Rodney girls' soccer team glad to be back on track

Dover's Velazquez overcomes injury to return to the mound

Photo gallery: Caesar Rodney vs. Smyrna girls' lacrosse

Former Blue Hen Davis headed for Syracuse
More Sports