Delaware State University addresses concerns after deadly shooting
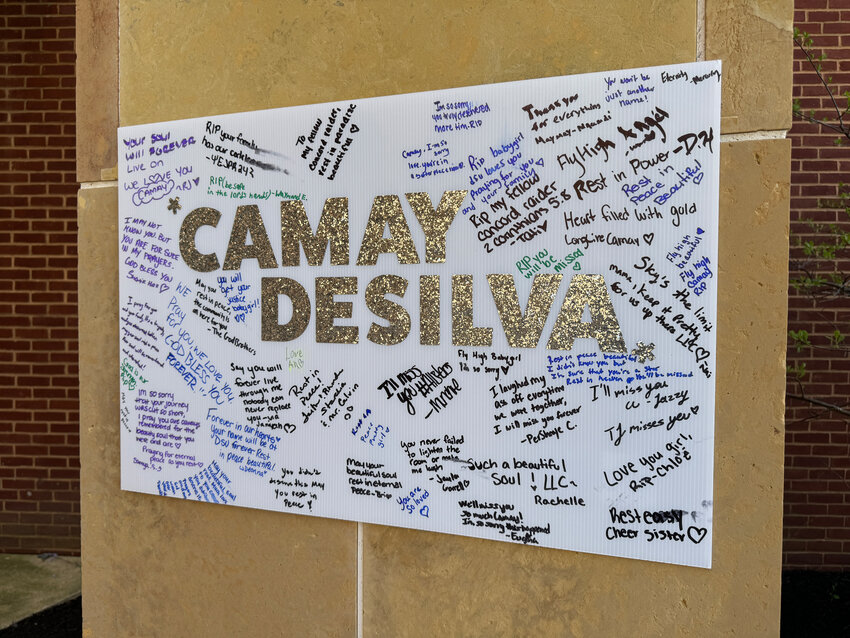
In the wake of Sunday’s deadly shooting at Delaware State University in Dover, which took the life of 18-year-old Camay DeSilva of Wilmington, school officials hosted a student forum Tuesday to speak about worry among community members.
-
-
Dover Police investigating Delaware State University Shooting that resulted in the death of an 18-year-old woman
DOVER -- The Dover Police Department says it is investigating a shooting that took place at its Dover campus early Sunday morning. …
-
-
-
Delaware Division of Small Business, Small Business Development Center partner to support business owners seeking loans
DOVER — The Delaware Division of Small Business is partnering with the Delaware Small Business Development Center to provide additional …
-
-
-
Delaware Forest Service joins Daughters of the American Revolution to establish Memorial Forest in Sussex County
The Delaware Forest Service hosted the Daughters of the American Revolution, Col. John Haslet Chapter in Dover, and other volunteers to …
-
-
Horton the Elephant, Yertle the Turtle, The Grinch and, of course, The Cat in the Hat will be on hand this weekend as The Children’s Theatre presents “Seussical: The Musical Jr.” at the Schwartz Center for the Arts in Dover.



View this issue of The Delaware State News or browse other issues.
Disclosure
-
-
Speak Up: How will cannabis commerce change Delaware?
Marijuana businesses are on their way to the First State, after the substance’s legalization for recreational use last year. What are your …
-
-
-
Speak Up: Gubernatorial candidate Meyer unveils plan to improve education
New Castle County Executive and gubernatorial candidate Matt Meyer has unveiled a comprehensive, 23-page education plan that focuses on remedies …
-
-
-
Speak Up: Delaware’s June Jam CEO, founder Hartley dead at 68
Bob Hartley, CEO and president of the June Jam charity music festival, died in his sleep April 14. Lynn Fowler, executive vice president of the …
-
-
M&D Bird Farm flies high in Harbeson
HARBESON — There are things one might expect when driving the roads of Sussex County. Construction is likely. Traffic might be a definite, depending on where you are. But it’s not common …



Downstate Delaware high school scores
Majorca N posts first win at Harrington Raceway

Smyrna boys' lacrosse team set to put its 8-0 record to the test

College notes: Delaware State baseball enjoying win streak; Delaware adds basketball transfer

Downstate Delaware high school scores
More Sports