Bill to provide Medicaid coverage for pregnancy termination advances as Delaware General Assembly returns from break
DOVER — The General Assembly returned to the state capitol on Tuesday after a two-week spring recess, but missed no time getting back to work. With just over two months left of this …
-
-
Homeless Bill of Rights pulled from Delaware House committee's Wednesday agenda
DOVER — As lawmakers prepared to return from their two-week spring recess on Monday, the Bill of Rights for Individuals Experiencing …
-
-
-
Delaware's June Jam CEO, founder Hartley dead at 68
Bob Hartley, CEO and president of the June Jam charity music festival, died in his sleep Sunday.
-
-
-
Sussex County Council reverses previous zoning denial
In August 2023, County Council voted 3-2 to deny a conditional use application for a solar farm south of Frankford but reversed course Tuesday …
-
-
DOVER — This is the time of the year when Miles the Monster’s heart starts to beat a little louder and his pulse begins to race. While the NASCAR Cup Series competes at Talladega …



View this issue of The Delaware State News or browse other issues.
Disclosure
-
-
Lewis: Solutions needed after rash of shootings in Dover
As one of your Dover City Council members and chair of the Safety Advisory and Transportation Committee, I felt compelled to publicly express …
-
-
-
Goduti: Kennedy left vision for peace unfinished
Less than a week after her husband’s assassination in Dallas on Nov. 22, 1963, Jackie Kennedy granted an interview with esteemed political …
-
-
-
Moreno and Radesky: Online child safety laws could help or hurt
Society has a complicated relationship with adolescents. We want to protect them as children and yet launch them into adulthood. Adolescents …
-
-
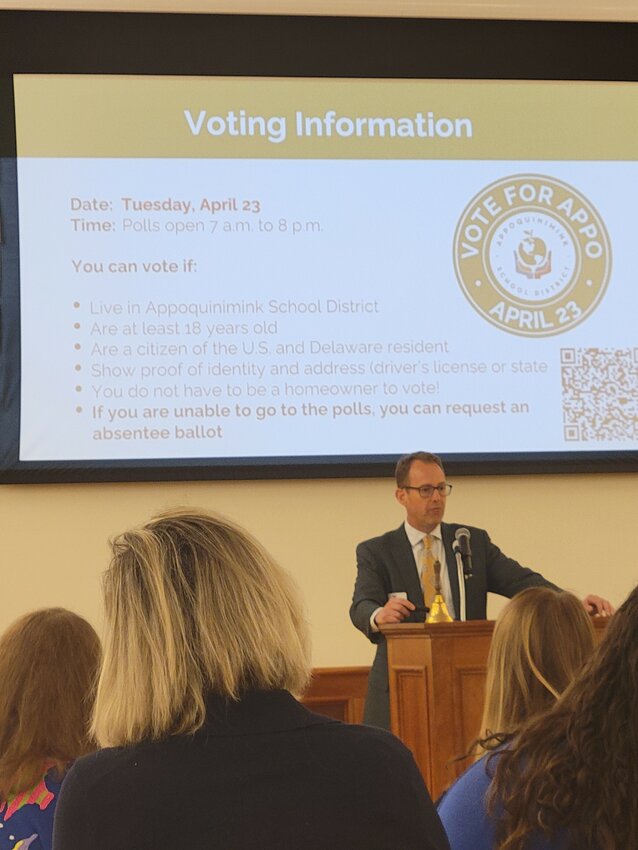
Middletown Area Chamber of Commerce holds spring luncheon
The Middletown Area Chamber of Commerce Spring Luncheon was held Wednesday at Middletown Memorial Hall.


College notes: Delaware State basketball team loses another standout but adds three transfers

Downstate Delaware high school scores

Harrington Raceway harness racing results

Photo gallery: Cape Henlopen vs. Caesar Rodney boys' lacrosse

Harrington Raceway harness racing results, entries
More Sports